Autores:
Introduction:
External tibial torsion is a bone deformity defined as any rotation of the tibia about its longitudinal axis. resulting in alteration in the planes of movement of the proximal and distal joints (11).
Rotational changes have a multifactorial origin stemming not only from congenital conditions but also, as LeDemanay (11) suggest, from muscular tension on the distal epiphysis of the tibia. This tension generates rotational stress, leading to abnormal torsion. Furthermore, rotational loads can be induced during walking (11)(12).
Normal tibial torsion values have been described in a range from 20 to 24 degrees of external rotation (11). Beyond these ranges, biomechanical repercussions on the knee occur: first, it mainly affects the patellofemoral compartment, explaining, in some cases, patellofemoral pain and, contributing to patellofemoral instability (8)(9)(10). Alteration in bone alignment result in changes to the patellofemoral displacement and can lead to ligament failure over time (26)
On the other hand, the contact pressures in the femorotibial spaces are affected; the greater the external tibial torsion is, the pressure increases in the external compartment and decreases in the internal compartment. This phenomenon occurs at both 15º and 30º of external rotation (11)(14).
In a previous study, carried out in 2011 by Kenawey et al (22), different results were obtained, indicating greater medial contact pressure with increasing external torsion of the tibia, without pressure changes in the lateral compartment. Additionally, they suggest that the decrease in femoral anteversion is also associated with an increase in contact pressure in the medial compartment. These changes ultimately lead to an increased risk of developing femorotibial osteoarthritis (OA) (11)(15)(16)(17)(18). Finally, not only the osteoarticular component is affected, but also the muscular capacity to extend the knee since the increase in external tibial torsion decreases the extension capacity of the posterior gluteus medius, gluteus maximus and soleus, contributing in cases to a gait with a flexed knee (23).
Due to the above, it is very important to carry out a comprehensive evaluation of each patient and this must have a clinical and imaging component. First, weight bearing anteroposterior, 30º lateral, and tangential patella radiographs are requested. Additionally, computed tomography (CT) with 3D reconstruction is requested and the methods of Murphy and Yoshioka (5)(6) are taken into account to measure femoral and tibial torsions. An alternative imaging method that offers advantages in terms of radiation exposure is biplanar radiography with the EOS system (Biomed, Paris, France). This method demonstrates reduced total radiation exposure (3 to 43 times versus CT (19); with no statistically significant differences observed in measurements when comparing biplanar radiographs versus 3D-2D CT (20)(21). Finally, magnetic resonance imaging should always be requested, as it allows the evaluation of associated ligamentous, chondral injuries. and/or meniscus.
During physical examination, Staheli tests (femoral anteversion), thigh-foot angles, and/or transmalleolar tests are used to evaluate rotational abnormalities. Additionally, the extended Q angle described by Manilov, allows not only the evaluation of rotational alterations of the tibia but also identifying associated alterations in the tibial tubercle trochlear groove (TT-TG) distance (3).
When the values fall outside the normal range, compensatory mechanisms from the pelvis to the foot come into play. However, this compensation primarily occurs at the hip and foot levels. Initially compensation occurs with internal rotation of the hip and an increase in the angle of foot progression (AFP), which is normally 4.5 degrees (+/- 8) (13). This translates into a gait with the knees pointing inward.
Once the decision to perform surgical correction of the excessive tibial torsion (>30º) is made, a proximal tibial osteotomy is performed, above or below the tibial tuberosity, depending on the need to modify the TT-TG, the objective is to improve the rotational profile, pain, patellofemoral instability (generally with associated procedures such as reconstruction of the medial patellofemoral ligament, among others) and improve functional results or PROMs (Patient related outcomes) (24). Additionally, it is important to perform the biplanar osteotomy since it generates greater stability in the anteroposterior and rotational planes according to cadaveric studies by Pape et al (25)
We find several benefits with this technique: firstly, the possibility of having additional and more precise control over the planned correction angle before the procedure, without compromising the stability of the osteotomy and ensuring complete contact between tibial tubercle (TT) and the adjacent proximal tibia, thereby reducing the risk of potential issues with bone consolidation, visualization of the complete proximal tibial bone surface and patellar tendon without muscle tissue (unlike lateral approaches for proximal tibial osteotomy). However, it's important to note that for osteotomies requiring a correction exceeding 30º, a lateral incision is performed to release the external popliteal sciatic nerve (EPSN). Additionally, a transverse osteotomy in the fibula is carried out to provide greater rotational freedom and reduce tension on the EPSN (1)
Technique:
Preoperative planning:
A malalignment test (MAT) is performed on a whole leg radiography (WLR) with the help of the application Bone Ninja (International center for Limb Lengthening, Sinai Hospital of Baltimore. LifeBridge Health) and the following calculations are made:
- MAD (mechanical axis of deviation)
- JLCA (joint line convergence angle)
- Mechanic Lateral distal femoral angle (mLDFA - Lateral distal femoral angle) and medial proximal tibial angle (MPTA - medial proximal tibial angle)
Additionally, tomography is used to assess femoral anteversion (following Murphy's method (5)) and tibial torsion (based on Yoshioka's method (6)), along with the calculation of the TT-TG distance. Finally, magnetic resonance imaging is employed to evaluate associated injuries in ligaments, meniscus, and articular cartilage.
Surgical Procedure:
- Spinal anesthesia and epidural catheter placement
- Supine position with lateral and distal support to keep the knee flexed in 90º.
- Arthroscopic evaluation and management of chondral, ligamentous, or meniscal pathologies.
- An anteromedial incision is made longitudinally at the proximal portion of the tibia.
- Dissection of the subcutaneous cellular tissue through the proximal tibial surface, pes anserinus and patellar tendon’s insertion.
- Biplanar marking of the osteotomy (above or below the TT depending on the need to correct (TT-TG) distance.
- A longitudinal incision is made posterior to the superficial medial collateral ligament (MCL), parallel to the fibers of the MCL (posterior Window).
- Subperiosteal dissection of the tibia’s posterior surface with a blunt dissector and then positioning a retractor to protect the popliteal neurovascular bundle.
- A 2.0 mm pin marks the transverse osteotomy direction, above the pes anserinus insertion and perpendicular to the anatomical axis of the tibia.
- Two 4.5 mm bicortical Schanz pins are inserted parallel to each other, perpendicular to the anterior tibial surface, both above and below the level of the osteotomy. These pins serve as a reference for rotation.
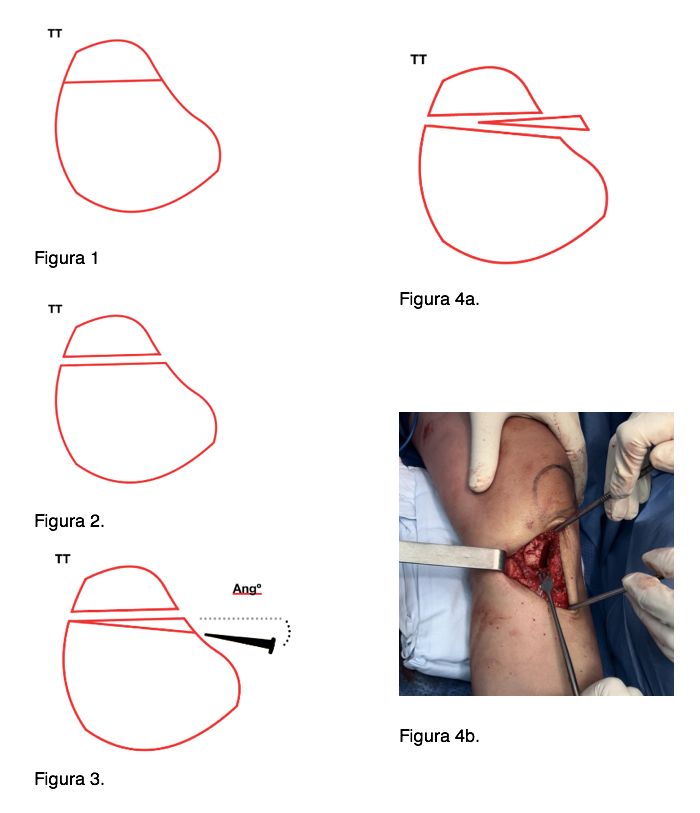
- The biplanar cut is performed with an oscillating saw and the osteotomy is completed with an osteotome (Figure 1 and 2).
- A longitudinal wedge of medial base is marked parallel to the anterior surface of the tibia. This marking is established using the lateral apex of the wedge and the anterior surface of the previous tibial cut as references. By incorporating the desired correction angle, the measurement of the anterior wedge resection magnitude is determined (Figure 3)
- The anterior wedge is cut with an oscillating saw and osteotome.
- Extraction of the resulting bone fragment (Figure 4a-b).
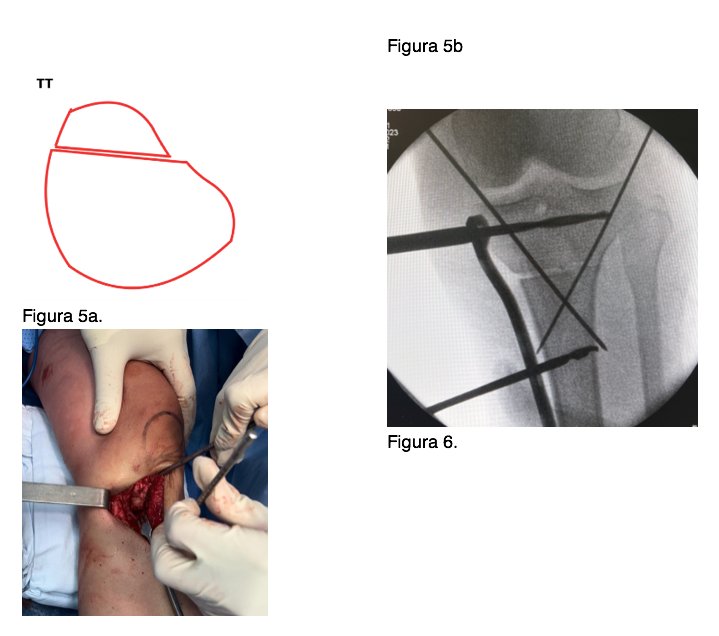
- Medial rotation of the tibia until reaching the predicted correction degrees, checking the latter with a goniometer. We observe that because of the wedge’s resection described previously, the TT remains in full contact and compression with the anterior tibial surface (Figure 5a-b).
- For temporary fixation, two 2.0 mm pins from each tibial plateau edges are used, aiming distally in crossed configuration (Figure 6).
- Definitive fixation with a Tomofix plate (DePuy Synthes, Solothurn, Switzerland) on the proximal and medial tibial surface.
- Lavage with saline solution, hemostasis and closure with vicryl and prolene.
- Wound dressing and thromboembolism prophylaxis in the form of low-molecular-weight heparin and antiembolic stockings.
- Postoperative x-rays, transition to the hospital room and guided physiotherapy with partial support with a walker.
- Discharge from hospital after 48 hours, doctor's office appointment after one month and radiographic control after 2 months.
Results:
Results obtained from the supra tubercular tibial derotational osteotomy procedure in a study carried out by Manilov (1) that show functional improvements on Kujala, Fulkerson-Shea scales (Images are taken from the original article).

Pre- and post-operative results, Kujala and Flukerson-Shea scores.
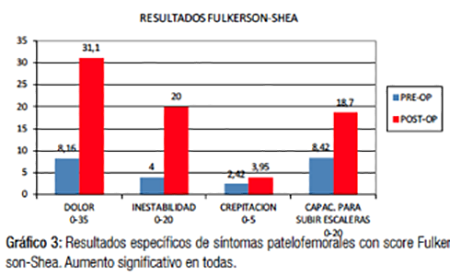
Specific patellofemoral symptoms results, Fulkerson-Shea score. Significant improvement in all variables.
References.
- Manilov, R. Osteotomía desrotadora supratuberositaria de tibia para mal alineación patelofemoral. Técnica bajo asistencia artroscópica. Artroscopia Vol 18, Nº 3: 132 - 141 (2011)
- Tuner MS, Smillie IS. The effect of tibial torsion of the pathology of the knee. J Bone Joint Surg Br 1981; 63:396-8.
- Manilov, R. Ángulo Q Extendido. Un Nuevo Signo Clínico para Decidir Técnica de Realineación Distal del Aparato Extensor. ARTROSCOPIA | Vol. 20, Nº 3 : 104-107 (2013)
- Staheli LT, Corbett M, et al. Lower-extremity rotational problems in children. Normal values to guide management. J Bone Joint Surg Am. 67:39-47.
- Murphy SB, Simon SR, et al. Femoral anteversion. J Bone Joint Surg Am 1987;69:1169-76.
- Yoshioka Y, Siu D, et al. Tibial anatomy and functional axes. J Orthop Res 1989;7:132-7.
- Fouilleron N, Marchetti E, et al. Proximal tibial derotation osteotomy for torsional tibial deformities generating patello-femoral disorders. Orthopaedics & Traumatology: surgery & research (2010) 96, 785-792.
- Walton DM, Liu RW et al. Proximal tibial derotation osteotomy for torsion of the tibia: a review of 43 cases. Journal of children’s orthopaedics, vol. 6. no. 1, pp. 81-85, 2012.
- Cameron JC, Saha S. External tibial torsion. Clinical Orthopaedics and related research, vol328, pp. 177-184, 1996.
- Wyatt P, Satalich J, et al. Tibial derotational osteotomy for patellofemoral instability: A systematic review. Advances in orthopaedics. Vol 2022
- Snow M. Tibial torsion and patellofemoral pain and instability in the adult population: current concept review. Current reviews in musculoskeletal medicine, vol. 14, no. 1, pp. 67-75, 2021.
- Yang PF, et al. On the relationship between tibia torsional deformation and regional muscle contraction in habitual human exercises in vivo. J Biomech. 2015 Feb; 48 (3):4566-64.
- Hudson D. The rotational profile: a study of lower limb axial torsion, hip rotation, and the foot progression angle in healthy adults. Gait Posture. 2016;49:426–30
- Yazdi H, Mallakzadeh M, et al The effect of tibial rotation on knee medial and lateral compartment contact pressure. Knee Surg Sports Traumatol Arthrosc. 2016 Jan;24(1):79–83.
- Turner MS. The association between tibial torsion and knee joint pathology. Clin Orthop. 1994 May;302:47–51.
- Yagi T. Tibial torsion in patients with medial-type osteoarthrotic knees. Clin Orthop. 1994;302:52–6.
- Bombaci H. Tibial torsion: cause or consequence of osteoarthritis? Acta Orthop Traumatol Turc. 2012;46(3):181–5.
- Tamari K, Briffa NK, et al. Variations in torsion of the lower limb in Japanese and Caucasians with and without knee osteoarthritis. J Rheumatol. 2007 Jan;34(1):145–50.
- Shih YC, ChauMM, et al. Measuring lower extremity rotational alignment: a review of methods and case studies of clinical applications. J Bone Jt Surg. 2020;102(4):343–56
- Buck FM, Guggenberger R, et al. Femoral and tibial torsion measurements with 3D models based on low- dose biplanar radiographs in comparison with standard CT measurements. AJR Am J Roentgenol. 2012;199:607–12
- Yan W, Xu X et al. Femoral and tibial torsion measurements based on EOS imaging compared to 3D CT reconstruction measurements. Ann Transl Med. 2019;7(18):460–0.
- Kenawey M, Liodakis E, et al. Effect of the lower limb rotational alignment on tibiofemoral contact pressure Knee Surg Sports Traumatol Arthrosc (2011) 19:1851–1859
- Hicks J, Arnold A, et al. The effect of excessive tibial torsion on the capacity of muscles to extend the hip and knee during single-limb stance Gait Posture. 2007 October ; 26(4): 546–552.
- Wyatt P, Satalich J, et al. Tibial Derotational Osteotomy for Patellofemoral Instability: A Systematic Review. Advances in Orthopedics Volume 2022.
- Pape D, et al. Effect of a biplanar osteotomy on primary stability following high tibial osteotomy: a biomechanical cadaver study. Knee Surg Sports Traumatol Arthrosc (2010) 18:204-211.
- Teitge, RA. Patellofemoral syndrome a paradigm for current surgical strategies. Orthop Clin N Am 39 (2008) 287 - 311.
Descargar versión en PDF
Proximal Tibial Biplanar and Derotation Osteotomy with Anterior Wedge Resection

